Soula Priovolos, MD, FACS
- Assistant Professor of Clinical Surgery
- Weill Medical College of Cornell University
- Lincoln Medical and Mental Health Center
- Bronx, New York
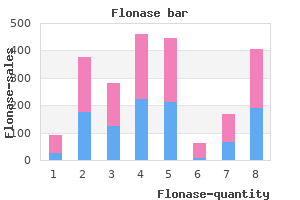
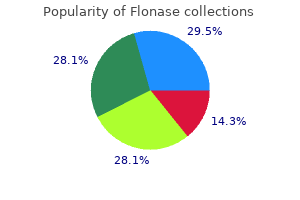
However allergy medicine grass pollen order 50 mcg flonase with mastercard, there were early concerns that nonanatomic or wedge resections as opposed to strictly anatomic operations based on one or more portal pedicles might be associated with higher blood loss and greater risk of bile leak allergy testing on dogs best flonase 50 mcg. For example, Zorzi and colleagues (2006) retrospectively reviewed 300 hepatic resections in 253 consecutive patients who underwent either wedge or anatomic hepatic resection for colorectal liver metastases over a 13-year period. Anatomic resections included segmentectomies, multisegmentectomies, sectionectomies, or segmentectomy plus sectionectomy (see Chapter 2) and were performed for large, deeply situated, or multiple clustered metastases; wedge resection was performed for small, peripheral, and isolated metastases. Median length of stay for both groups was 7 days; there was only one postoperative death after wedge resection (1. By reducing liver failure and decreasing the physiologic impact of surgery, parenchymal-preserving techniques maximize the patient population eligible for surgery. Unfortunately, many patients with malignant hepatic tumors are not candidates for resection because of underlying liver disease or the extent of tumor burden. This includes patients whose liver function will not permit a formal hepatic resection and those with bilobar disease or anatomically challenging lesions such as those deep, centrally located, or involving or threatening major vasculature. These situations can be common in the population referred for surgical evaluation. Zorzi and colleagues (2006), in their review of 300 hepatic resections for colorectal cancer metastases, noted that 43% of patients had multiple metastases and 12% underwent more than one wedge or anatomic resection at surgery. Although they did not comment on the number of patients who would have been ineligible for surgery if parenchymal-sparing techniques had not been employed, this report and other data suggest that a large number of patients stand to benefit from techniques that preserve liver parenchyma and/or allow multiple synchronous resections or staged operations. Biochemical definition of liver dysfunction based on hyperbilirubinemia, elevated serum ammonia, and prothrombin time prolongation. Treatment: Resection Chapter 108A Parenchymal preservation in hepatic resectional surgery: rationale and indications 1635 likely have been ineligible for surgery. While demonstrating the safety of parenchymal-preserving techniques for resection of primary and secondary hepatic malignancy, it is imperative that surgeons demonstrate that these techniques preserve oncologic principles of removing tumor and tumor-bearing tissue with a sufficient margin and in a manner minimizing the risk of local recurrence (see Chapters 103A and 103B). Colorectal liver metastases are histologically wellcircumscribed (Yamamoto et al, 1995). Micrometastases in the surrounding liver parenchyma are rare and primarily found at the immediate tumor border, and satellitosis and Glisson sheath extension are uncommon (Kokudo et al, 2002; Scheele et al, 1995). The series included patients who underwent an extended hepatectomy (18%) and hemihepatectomy (39%), as well as lesser resections. Patients were classified into four subgroups according to the width of the resection margin: positive (tumor <1 mm from surgical margin) or negative (by 1-4, 4-9, or at least 10 mm). With a median follow-up of 29 months, 225 of the 557 patients developed a recurrence (40%). A positive resection margin affected disease-free survival, but sites and incidence of recurrence were similar among patients with a negative margin of resection, regardless of the width of the margin. Median survival also did not differ based on whether the patient underwent an extended hepatectomy, a hemihepatectomy, or less than a hemihepatectomy. In a separate study, oncologic outcomes were examined in a subset of these patients (n = 253) undergoing less than a 1. Survival after hepatic resection of colorectal liver metastases, stratified by margin status. No significant difference in survival was seen in patients with a negative surgical margin, regardless of the width of the margin (all P >. Operative goals were to resect all disease with a margin of microscopically normal tissue. The incidence of isolated intrahepatic recurrence after a wedge resection was only 14% compared to 9% after an anatomic resection (P =. Recurrence at the surgical margin was more common in patients who had a positive resection margin regardless of the type of resection, but margin positivity was equivalent between the groups. The goal of either surgical approach was to removal all intrahepatic tumors with sufficient margins. In a subset analysis of patients with unilobar disease, the authors noted an ipsilateral intrahepatic recurrence rate of 19. Moreover, 90% of patients who had tumor recurrence in the hepatic lobe ipsilateral to their original surgery were resectable in a second operation, with a 5-year survival rate of 58. Recurrences were much less likely to be resectable (20%) among those undergoing more extensive, anatomically based resections (of whom half required hemihepatectomy to clear their initial disease). In this series, operative morbidity and mortality were slightly higher in the anatomic resection group, a finding that was not borne out by the multiinstitutional study (Pawlik et al, 2005; Zorzi et al, 2006). They reported similar overall survival between the two groups and repeat hepatectomy more often after parenchymal-sparing hepatectomy. In the subset of patients who had recurrence in the liver only, anatomic resection was an independent factor of noncandidacy for repeat hepatectomy, and the survival was significantly better in the parenchymal-sparing hepatectomy group. The same appears true for other secondary malignancies of the liver (Billingsley et al, 1998). Although no study has specifically evaluated the prognostic value of margin width, we and other investigators have found that surgical resection versus resection and ablation versus ablation alone does not significantly influence outcomes (Mayo et al, 2010; Saxena et al, 2011). In contrast, anatomic resections that remove the hepatic segment defined by tumor-bearing (Agrawal & Belghiti, 2011; Liau et al, 2004). Five-year disease-free and overall survival were 67% and 28%, respectively, in the segmentectomy and subsegmentectomy group and 35% and 16% in the group undergoing limited resection. The authors attempted to control for this imbalance using multivariable Cox proportional hazards model accounting for other prognostic factors and still found that anatomic versus nonanatomic resection carried a favorable survival benefit. In 2008, Eguchi and colleagues reported long-term results from the Liver Cancer Study Group of Japan, which has been conducting nationwide surveys of patients with primary liver cancer since 1969. With a median follow-up of over 2 years, overall survival appeared to favor anatomic resection (34% survival at 10 years vs. However, diseasefree survival was highest among patients who underwent anatomic resection (40% vs. In these two other studies, choice of operative strategy rested with the surgeon, and minor/nonanatomic hepatectomy was performed more frequently in patients with impaired liver function. Therefore, the definitive nature of survival outcomes in this and other inherently biased retrospective studies (Fuster et al, 1996; Imamura et al, 1999) has been questioned by authors who believe that an uncompromising anatomic resection is not strictly necessary to achieve oncologic goals (Ahn et al, 2013; Torzilli et al, 2005). However, the rationale behind performing anatomically based but parenchymal-sparing operations over more extensive resections must include demonstration that parenchymal-sparing techniques do not put the patient at an oncologic disadvantage by failing to remove "at risk" tissue that can be the source of tumor recurrence. Others have demonstrated similar disease-free and overall survival rates after parenchymal-preserving versus hemihepatectomy and more extensive resections (Kosuge et al, 1993; Imamura et al, 1999; Okada et al, 1994), suggesting that when a margin-negative resection can be achieved by a parenchymal-sparing segmental resection, more extensive operations do not proffer a survival advantage. Surgical approach was based entirely on preoperative evaluation of tumor extent: local E. Extended right or left hepatectomies (n = 66) were performed for lesions invading beyond the confluence of the bile ducts. The vast majority (93%) of segmental resections could be performed with a microscopically clear margin, and 71% of extended resections were margin negative. However, local excision in this series carried a dismal 62% rate of margin positivity and was associated with a poor, 8% 5-year overall survival. Of note, extended hepatectomy was associated with significantly higher morbidity (48% vs. Parenchymal-preserving techniques allow for second, "salvage" operations and for planned two-stage strategies. Although the liver has a substantial regenerative capacity, patients who have undergone one major resection often do not have enough remaining hepatic parenchyma to allow a second extensive operation. Thus, a more conservative initial resection maximizes the possibility of repeated resections if patients develop new lesions, which are more likely to occur in areas of the liver other than the site of the previous tumor (Billingsley et al, 1998), and for which repeat resections can significantly extend patient survival (Muratore et al, 2001; Nakajima et al, 2001; Suzuki et al, 2001Yamamoto et al, 1999). In patients undergoing segmental resection for hepatic neoplasm at a single institution, 18 of the 79 patients were undergoing a second operation (Billingsley et al, 1998). In select patients with multifocal, bilobar metastases not amenable to a single hepatectomy procedure, two-stage hepatectomy may yet offer a chance for long-term remission (Adam et al, 2000, 2007; Jaeck et al, 2004; Shimada et al, 2004; Togo et al, 2005; Wicherts et al, 2008). After an interval during which patients typically receive chemotherapy, patients are restaged and the contralateral lobe resected with curative intent. A, Overall survival, and B, disease-free survival, after hepatic resection for single hepatocellular carcinoma, stratified by type of resection. C and D, Overall survival after hepatic resection for colorectal liver metastases, stratified by surgical procedure.
Diseases
- Metaphyseal dysostosis mental retardation conductive deafness
- Delta-1-pyrroline-5-carboxylate dehydrogenase deficiency
- Premature aging, Okamoto type
- Lactic acidosis congenital infantile
- Histiocytosis X
- Rhinotillexomania
A second meta-analysis published the same year allergy partners of richmond discount flonase 50 mcg line, however food allergy symptoms quiz purchase flonase overnight, did incorporate the results from that study and found an absolute survival difference of 12. Irinotecan is a topoisomerase I inhibitor with proven efficacy in first-line and second-line treatment of metastatic colorectal cancer. The regimen was well tolerated, with dose-limiting toxicities of diarrhea and myelosuppression. Seventy-one patients received "adjuvant" therapy and were compared with a historic control group that received cytoreduction alone. Oxaliplatin is a cytotoxic agent with a mechanism of action similar to that of other platinum derivatives, but it has a different spectrum of activity and toxicity. Both regimens were well tolerated, and response rates for the two groups were 90% and 87% (see Table 99. A partial or complete response was reported in 92% (84% partial, 8% complete), and 47% of patients were able to undergo resection, 3 with pathologic complete responses. Twenty-three patients (47%) achieved conversion to resection in a median of 6 months from treatment initiation. Neoadjuvant treatment is a strategy increasingly used in solid-tumor oncology, given the multifaceted rationale that it may enable downsizing and subsequent resectability of tumor burden. Recurrence may be solely in the liver, it may be extrahepatic and intrahepatic, or it may be solely extrahepatic. An effective adjuvant treatment may have a substantial impact on recurrence and survival. Forty percent of patients received prior adjuvant chemotherapy after resection of their primary colorectal cancer, and 15% had received prior chemotherapy as treatment for metastatic disease. Randomization was performed intraoperatively after complete resection of metastases, and patients were stratified based on number of metastases and prior treatment history. In an updated analysis, with all patients followed for a minimum of 6 years (median follow-up, 10. Median survival free of hepatic progression had not yet been reached in the combined-therapy group but was 32. Toxicity was increased in the combined group, and 39% of patients required hospitalization for diarrhea, neutropenia, mucositis, or small bowel obstruction, compared with 22% in the monotherapy group (P =. In most patients, the bilirubin returned to normal, but 6% of patients required biliary stents. In the control group, 2% had an elevation in bilirubin, and 2% required biliary stents. Not reported, but calculated based on Kaplan-Meier curves published in original citations. A score ranging from 0 to 5 was calculated by adding 1 point for the following clinical variables: tumor size > 5 cm, tumor number > 1, serum carcinoembryonic antigen > 200 ng/mL, node-positive primary tumor, and diseasefree interval > 12 months. The study was terminated early because an interim analysis suggested a very low chance of showing a survival benefit with adjuvant therapy. When patients were analyzed "as treated," time to hepatic progression (45 months vs. Grade 3 or 4 toxicity, including stomatitis, nausea, and vomiting, was noted in 63% of patients who received adjuvant therapy. Historic 2-year survivals (Chang et al, 1987; Fegiz et al, 1991; Jamison et al, 1997; Scheele et al, 1990) for patients treated with resection alone range from 55% to 70%. The dose-limiting toxicities were diarrhea and neutropenia, and all 27 patients treated at the maximum-tolerated dose were alive at publication (Kemeny et al, 2003). In fact, hyperbilirubinemia greater than 3 mg/dL occurred in five patients in the bevacizumab arm, with four requiring placement of biliary stents. One patient in this study responded sufficiently to undergo resection and was found to have had a complete pathologic response. The median duration of response was 1 year, and median time to progression was 7 months. Median follow-up at time of publication was 35 months, and 1- and 2-year survival was 88% and 67%, respectively. Treatment: Nonresectional Chapter 99 Regional chemotherapy for liver tumors 1487 correlated with median survival, which may therefore serve as biomarkers of treatment outcome. Arai Y, et al: Interventional techniques for hepatic arterial infusion chemotherapy. Harmantas A, et al: Regional versus systemic chemotherapy in the treatment of colorectal carcinoma metastatic to the liver: is there a survival difference Ito H, et al: Effect of postoperative morbidity on long-term survival after hepatic resection for metastatic colorectal cancer.
Chapter 113 Liver transplantation: anesthesia allergy zyrtec buy flonase on line amex, perioperative management allergy medicine yellow pill flonase 50mcg mastercard, and postoperative care1765. Taner C, et al: Is a mandatory intensive care unit stay needed after liver transplantation It results from overwhelming death of hepatocytes of varied etiology exceeding the regenerative capacity of the liver and results in the development of a potentially life-threatening condition that presents most often in a patient without cirrhosis or preexisting liver disease. If left untreated, the prognosis is poor, with mortality rates exceeding 85% (Bernuau et al, 1986; Riordan et al, 2008). At present, however, mortality has fallen to approximately 30% to 35%, with 20% to 25% of patients requiring emergency liver transplantation, and 40% to 45% of patients able to survive spontaneously because of advances in their intensive care management (Lee et al, 2008; Ostapowicz et al, 2002; Polson, 2008). Because of this low frequency and patient heterogeneity, supportive care in these patients has often been anecdotal, with limited level 1 evidence to guide clinical care. However, certain strategies have become well established and their benefits widely proven. French investigators have highlighted the importance of recognizing the syndrome even at an earlier stage, that is, as soon as prothrombin ratio falls below 50% and before the development of encephalopathy, emphasizing that prompt referral to a specialized liver unit and rapid medical intervention with specific therapies in certain etiologies can prevent the progression of the clinical picture and improve survival (Bernuau, 1993). Once altered mental status develops, clinical deterioration may be very rapid, so immediate contact with a transplant center should occur, to determine whether transfer is appropriate. Sedation should be avoided because it may mask the signs of worsening encephalopathy or cerebral edema. In patients who are severely agitated, short-acting benzodiazepines may be given with caution. This suggests a balanced hemostatic defect, in which the loss of hepatic synthesis of procoagulant factors is paralleled by the loss of liver-derived anticoagulants, making spontaneous bleeding uncommon (Agarwal et al, 2012). Etiologic screening should include viral serologies, circulating acetaminophen levels, screens for other drugs and toxins, tests for Wilson disease, autoantibodies, and pregnancy tests for women (Box 114. It remains mandatory that all nonessential medications should be discontinued (Lee et al, 2011). In patients with suspected or known acetaminophen overdose, early activated charcoal may be useful for intestinal decontamination (within as long as 4 hours of ingestion). N-acetylcysteine should also be given as soon as possible, although it may still be of value even 48 or more hours after ingestion of acetaminophen (Green et al, 2001; Sato et al, 2003). When etiologic diagnosis remains elusive after extensive initial evaluation, liver biopsy through a transjugular approach may be appropriate, to attempt to identify a specific cause that might impact treatment strategy, such as malignant infiltration precluding transplantation, autoimmune hepatitis, certain viral infections, and Wilson disease (Miraglia et al, 2006; Singhal et al, 2012). Etiologies vary in adults compared with infants and children (Ostapowicz et al, 2002; Polson et al, 2005; Squires et al, 2006), and relative frequency of etiologies show geographic (Lee, 2008) and temporal variations. These variations depend mainly of epidemiologic, socioeconomic, and cultural issues. High prevalence of autoimmune hepatitis, as reported in Argentina and other Latin American countries, remains unexplained (Gerona & Cohen [Uruguay]; Clinica Alemana [Chile], personal communication), even though it correlates with a high proportion of patients transplanted for autoimmune disease (also among patients with cirrhosis), suggesting a more severe course of autoimmune liver disease. Drug toxicity may be dose dependent and predictable, as with acetaminophen, or idiosyncratic and unpredictable, as with other medications. In a recent analysis of 1033 patients enrolled through 2007, acetaminophen toxicity accounted for approximately 46% of cases, followed by indeterminate origin (15%) and idiosyncratic drug reactions (12%). In the remainder, ingestion results from unintentional overuse of acetaminophencontaining compounds for pain or fever relief at therapeutic doses, mainly by patients with ongoing alcohol abuse. Other compounding factors include starvation or concurrent use of medications known to induce the cytochrome P450 system, such as anticonvulsants, a situation known as "therapeutic misadventure" (Licht et al, 1980; Seeff et al, 1986; Wootton & Lee, 1990). Risk of death is directly related with substantial drug ingestion during hours or days, rather than at a single time point. Although the case fatality of this syndrome is lower than that observed with suicidal ingestion, it is still at least 20% in most reviews (Kumar et al, 1991; Wootton & Lee, 1990). It is important that ingredients of nonprescription medications be determined whenever possible. Strict inquiry should also include herbal preparations, weight loss agents, and other nutritional supplements (Lee et al, 2011).
The physiological effects are geared toward satisfying increased tissue O2 and energy requirements and concomitant cardiovascular demand allergy treatment ramdev order cheap flonase on line. Both heart rate and cardiac contractility are increased to elevate cardiac output allergy symptoms of mold buy flonase 50mcg lowest price, blood flow is shifted from internal organs not critical for fight-or-flight to skeletal muscle, and energy is made available via increased metabolism. Moreover, there are other physiological changes pertinent to fight or flight, such as bronchodilation and activation of sudomotor pathways. Drugs that facilitate or mimic the actions of the sympathetic nervous system are called sympathomimetics, adrenomimetics, or adrenergic agonists. Sympathomimetics may exert their effects by binding directly to adrenergic receptors (direct acting;. These drugs are generally used clinically for disorders in which mimicking the fight-or-flight response helps to improve the condition or provide relief for the underlying disease. The therapeutic use of these sympathomimetics is primarily dictated by the specific receptor subtype(s) with which they interact. Adrenergic agonists are useful in a variety of clinical settings, ranging from treatment of cardiogenic shock to palliative treatment in asthma. This article will discuss the physiological effects of activating different adrenergic receptor types, the drugs that act on these receptors, and the therapeutic uses of these drugs. Of these, only four receptors (1, 2, 1, and 2) are important in current clinical pharmacology. In contrast, propranolol, a competitive antagonist at both 1 and 2 receptors, causes a parallel shift to the right of responses mediated by both cardiac 1 receptors and bronchial 2 receptors without affecting the 1 receptor response. Unlike drugs that activate 1- and -adrenergic receptors, agonists at 2-adrenergic receptors reduce sympathetic tone and are sympatholytic. Drugs that activate 2-adrenergic receptors, such as clonidine and guanfacine, are beneficial when a reduction in the fight-or-flight response is warranted. Thus activation of 2-adrenergic receptors reduces heart rate and promotes vasodilation, beneficial for the management of hypertension. A summary of the primary uses of different classes of compounds that affect the sympathetic nervous system is presented in the Therapeutic Overview Box. Direct-acting adrenergic receptor agonists mimic some of the effects of sympathetic nervous system activation by binding to and activating specific receptor subtypes. Agonists selective for 1 receptors include phenylephrine and methoxamine, while agonists selective for 2 receptors include clonidine and guanfacine. Conversely, the noradrenergic system can be inhibited by directly stimulating presynaptic feedback receptors with 2 agonists. Muscles were incubated with progressively increasing concentrations of each compound, and changes in the force of contraction (arterial and heart muscle) or relaxation (bronchial muscle) were measured. Muscles were incubated with progressively increasing concentrations of each compound in the absence or presence of a fixed concentration of the -receptor antagonist phentolamine or the -receptor antagonist propranolol. Changes in the force of contraction (arterial and heart muscle) or relaxation (bronchial muscle) were measured. Data suggest that ephedrine likely activates only -adrenergic receptors in humans, while pseudoephedrine may be activating both - and -adrenergic receptor subtypes. Baroreceptors are mechanosensors that respond to stretch and are located in the walls of the heart (atria and right ventricle), blood vessels (pulmonary vessels, carotid sinus, aortic arch), and the juxtaglomerular apparatus. An elevation in blood pressure increases the firing rate of these baroreceptor neurons that project to vasomotor centers in the medulla, decreasing the activity of these cells and concomitantly decreasing sympathetic outflow to the heart and blood vessels. In addition, the increased firing of the baroreceptor neurons increases vagal activity to the heart, decreasing heart rate. The clinical response to a drug reflects both the direct effects of the agent on effector organs and the reflex response. When an 1-adrenergic receptor agonist, such as phenylephrine, is administered, vascular smooth muscle contracts, increasing peripheral resistance and blood pressure. This increase in pressure elevates afferent baroreceptor neuronal activity, thereby reducing sympathetic nerve activity and increasing vagal nerve activity. Consequently, heart rate decreases (bradycardia), while peripheral resistance remains elevated because of the drug. In contrast, if a pure 1-adrenergic agonist is administered, heart rate and cardiac contractility increase, leading to an elevation in blood pressure. Activation of the baroreceptor reflex reduces sympathetic output, which decreases peripheral resistance. Thus while an increase in heart rate and cardiac contractility persist because of the drug, blood pressure decreases as the sympathetic tone to blood vessels is diminished. Thus drugs causing vasoconstriction will cause reflex slowing of the heart, whereas drugs increasing heart rate and contractility will promote a reflex vasodilation. Epinephrine the Cardiovascular System Epi is the prototype direct-acting sympathomimetic because it activates all known adrenergic receptors. By activating cardiac 1 receptors, Epi increases the strength, rate, and rhythm of cardiac contractions, actions that may be either desirable or undesirable. Epi increases the force of contraction (positive inotropic effect) by activating 1 receptors on cardiomyocytes and increases the rate of contraction (positive chronotropic effect) by activating 1 receptors on pacemaker cells in the sinoatrial node. Epi also accelerates the rate of myocardial relaxation (positive lusitropic effects) to shorten systole more than diastole. Thus the fraction of time spent in diastole is increased, allowing for increased filling of the heart. The combination of an increased diastolic filling time, more forceful ejection of blood, and increased rates of contraction and relaxation of the heart results in increased cardiac output. Epi also activates conducting tissues, increasing conduction velocity and reducing the refractory period in the atrioventricular node, the bundle of His, Purkinje fibers, and ventricular muscle. These changes and the activation of latent pacemaker cells may lead to alterations in heart rhythm. Large doses of Epi may cause tachycardia, increased cardiac muscle excitability, premature ventricular contractions, and ventricular fibrillation. These effects are more likely to occur in hearts that are diseased or have been sensitized by halogenated hydrocarbon anesthetics (Chapter 26). Vascular smooth muscle is regulated primarily by 1 and/or 2 receptors, depending on the location of the vascular bed. Epi is a powerful vasoconstrictor in vascular beds expressing primarily 1-adrenergic receptors, including arteries and arterioles in the skin, mucosa, brain, lungs, and abdominal viscera. However, it is a vasodilator in resistance vessels expressing primarily 2 receptors, particularly those in skeletal muscle. In veins, vascular beds such as those of the kidney and coronary arteries express both 1 and 2 receptors, and Epi leads to a mixed effect. Thus Epi increases blood flow in skeletal muscle but reduces flow in most other organs, consistent with the endogenous fight-or-flight function of Epi. While the vascular effects of Epi have a major impact on blood flow in organs, other factors also influence the clinical effect. For example, systemic administration of Epi alters cerebral and coronary blood flow, but the changes do not result primarily from direct actions of Epi on vascular smooth muscle. Rather, changes in cerebral blood flow reflect changes in systemic blood pressure, and increased coronary blood flow results from a greater duration of diastole and production of vasodilator metabolites. Other Smooth Muscle Epi is a potent bronchodilator, relaxing bronchial smooth muscle by activating 2 receptors. It dramatically reduces responses to endogenous bronchoconstrictors and can be lifesaving in acute asthmatic attacks (Chapter 72). The vasoconstrictor phenylephrine or the vasodilator histamine was administered intravenously and responses measured. Blood pressure (mm Hg) Vagus nerve activity (voltage arbitrary) Heart rate (beats/min) 100 100 40 0 Time (min) 1. Epi can foster urinary retention by relaxing the detrusor muscle and contracting the trigone and sphincter of the urinary bladder. The radial pupillary dilator muscle of the iris contains 1 receptors and contracts in response to activation of sympathetic neurons, causing mydriasis. However, such a response is not observed when Epi is applied topically onto the conjunctival sac of a normal eye.
Buy flonase 50mcg with amex. BABY ANNOUNCEMENT & FAMILY REACTIONS.
References
- Hirsch G, Kitas G, Klocke R. Intra- articular corticosteroid injection in osteoarthritis of the knee and hip: factors predicting pain relief- a systematic review. Semin Arthritis Rheum 2013; 42(5):451-73.
- Tabernero J, Hoff PM, Shen L, et al. 6160-pertuzumab (P) + trastuzumab (H) + chemotherapy (CT) for HER2- positive metastatic gastric or gastro-oesophageal junction cancer (mGC/GEJC): final analysis of a phase III study (JACOB). Ann Oncol 2017;28(Suppl 5):v209-v268.
- Yassa L, Cibas ES, Benson CB, et al. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer 2007;111(6):508-516.
- Rudy EB, Turner BS, Baun M, et al: Endotracheal suctioning in adults with head injury. Heart Lung 20:667, 1991.
- Effects of intensive diabetes therapy on neuropsychological function in adults in the Diabetes Control and Complications Trial. Ann Intern Med. 1996; 124(4):379-388.
- Lakhanpal S, Lie JT, Conn DL, Martin WJ 2nd. Pulmonary disease in polymyositis/dermatomyositis: a clinicopathological analysis of 65 autopsy cases. Ann Rheum Dis 1987;46(1):23-9.